When the the U.S. Food and Drug Administration (FDA) first approved the abortion medication mifepristone in 2000, prominent conservatives worried it might lead to an increase in abortions.
“I think the FDA’s decision to approve the abortion pill RU-486 [mifepristone] is wrong,” then-candidate George W. Bush said at the time. “I fear that making this abortion pill widespread will make abortions more and more common, rather than more and more rare.”
Fortunately for pro-life advocates, Bush’s fears only came true in part. While mifepristone itself has become more and more common—accounting for a majority of U.S. abortions by 2020—abortions overall have become more and more rare (albeit with an uptick during the Trump administration).
Regardless of where those trends go in the future, the Supreme Court’s June 24 decision in Dobbs v. Jackson Women’s Health Organization overturning Roe v. Wade will focus more attention on mifepristone in America’s ongoing conflict over abortion.
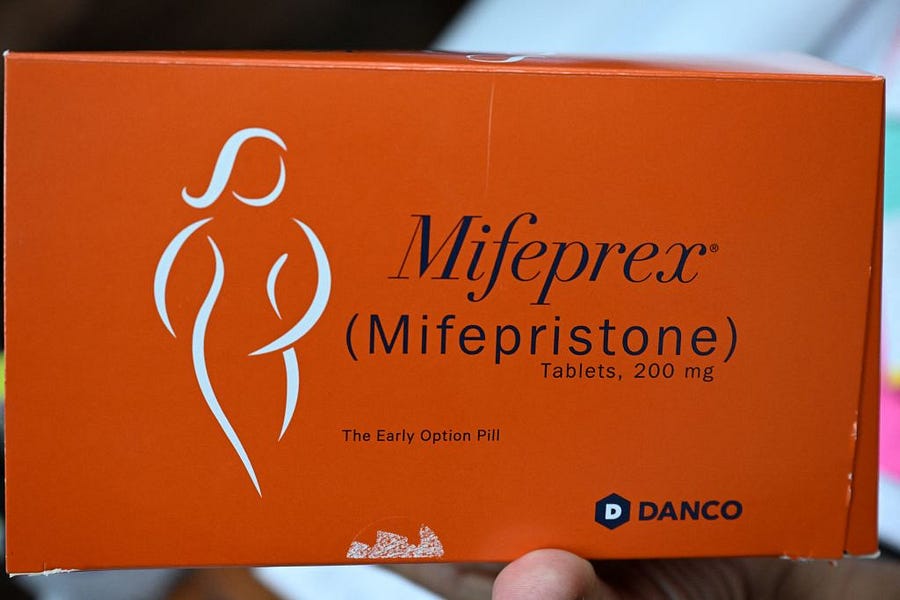
Mifepristone is the first part of a two-drug regimen approved by the FDA to induce abortion through the first 10 weeks of pregnancy. The regimen involves the patient taking a mifepristone pill followed by a dose of another drug, misoprostol, within 24-48 hours. Mifepristone blocks the hormone progesterone, killing the embryo or fetus. (In medical terminology, the developing baby is called an embryo through the first eight weeks of pregnancy and a fetus after that.) Misoprostol causes uterine contractions, inducing what is essentially a miscarriage. To distinguish it from surgical abortion, this process is typically referred to as medication abortion, though some pro-life groups use the term “chemical abortion” instead.
Although the FDA has only approved mifepristone for use through the first 10 weeks of pregnancy, it can also be prescribed for non-FDA-approved “off-label” uses in some states, but not others. A 2015 paper noted that, per World Health Organization recommendations, mifepristone and misoprostol are increasingly used for second-trimester abortions around the world, supplementing or replacing surgical methods. Greer Donley, a University of Pittsburgh law professor, told The Dispatch that it is “not uncommon” for mifepristone to be prescribed off-label up to at least 12 or 13 weeks in the United States.
But medication abortion can pose risks for the mother, especially after the 10-week mark. Dr. Donna Harrison, CEO of the American Association of Pro-Life Obstetricians and Gynecologists, pointed to a 2011 Finnish study which, while concluding that “medical TOP [termination of pregnancy] during the second trimester is generally safe,” showed elevated risks of infection and “surgical evacuation” of the uterus after 10 weeks.
Medication abortion is often confused with emergency contraception. Emergency contraceptives, such as Plan B, can be picked up over the counter and are designed to prevent pregnancy by halting ovulation, preventing fertilization, or preventing a fertilized egg from implanting in the wall of the uterus. In contrast, mifepristone requires a prescription from a certified provider and terminates the pregnancy after the fertilized egg has already implanted in the uterus.
For those in the pro-life community who believe human personhood begins at conception, this distinction between emergency contraception and medication abortion is a moot point: Preventing the implantation of a fertilized egg is still the taking of a life. As a result, some pro-life groups, such as Students for Life of America, consider Plan B an abortifacient drug.
Mifepristone is subject to a Risk Evaluation and Mitigation Strategy (REMS), a safety program the FDA “can require for certain medications with serious safety concerns to help ensure the benefits of the medication outweigh its risks.” Misoprostol is not.
According to the FDA, the REMS for mifepristone includes the following components:
Mifepristone must be prescribed by or under the supervision of a certified health care provider who meets certain qualifications, including signing a Prescriber Agreement Form.
The health care provider must obtain a signed Patient Agreement Form from the patient after counseling and prior to prescribing mifepristone.
Pharmacies that dispense mifepristone must be certified.
Before the COVID-19 pandemic, the REMS included an “in-person dispensing requirement.” During the pandemic—when non-emergency, in-person doctor’s appointments became a rarity—that requirement became the focus of a legal tug-of-war spanning both the Trump and Biden administrations. The Biden administration stopped enforcing it, first on a temporary basis in April 2021, and then permanently in December 2021. As a result, some mifepristone distribution began to take place through the mail.
A Harvard Law Review article on the subject called the changes to the REMS in 2021 “the most significant federal liberalization of medication-abortion access” to date.
But the sweeping federal policy changes belie the fact that there is a more complicated patchwork of policies at the state level. For example, according to the pro-choice Guttmacher Institute, “19 states require the clinician providing a medication abortion to be physically present when the medication is administered,” functionally eliminating the telemedicine consultation option for women seeking medication abortions in those states.
The end of Roe will only make that state policy patchwork more visible in the coming months and years. Imagine a state—say, Virginia—ends up banning abortions after 15 weeks but doesn’t pass any laws regarding mifepristone. Since mifepristone is only approved for the first 10 weeks of pregnancy, doctors and patients in Virginia could go on prescribing and using it as before.
In South Carolina, which currently bans most abortions after six weeks but has not attempted to outlaw mifepristone, the drug remains legal during the first six weeks of pregnancy, but not after (except in cases involving rape, incest, or danger to the life of the mother).
These scenarios would seem to point to a simple rule of thumb: When and where abortion is legal, mifepristone is legal—and when and where abortion is illegal, mifepristone is illegal.
But it’s not that simple. As mentioned above, some states have at least some laws addressing mifepristone that are more stringent than what the FDA’s REMS requires. For example, according to the Guttmacher Institute, about 30 states require the clinicians who administer the drug to be licensed physicians.
Right now, it’s hard to prevent women from acquiring abortion pills through the mail, even in states where abortion is fully banned—although Texas is trying. International companies such as the Dutch group Aid Access are continuing to send mifepristone to American women, which runs afoul of the REMS even in states where abortion is legal. The clandestine, self-managed abortions that result from these transactions are less safe than they might be under the REMS. In a 2017 survey of abortion and family planning providers, 35 percent of respondents said they had “witnessed complications from self-managed abortion with misoprostol/mifepristone,” and only half of providers said they thought using the two drugs for self-managed abortion was safe.
In 2020, the drugmaker GenBioPro, which produces generic mifepristone, sued Mississippi over its restrictions of mifepristone, which the company said “contravene federal law, are thus unconstitutional under the Supremacy Clause of the United States Constitution, and are preempted.”
Last week, both parties submitted written statements to the federal judge on the impact (or lack thereof) that the Dobbs decision may have on the case. While Mississippi argued that the state has clear authority under Dobbs to regulate abortion, GenBioPro cited Attorney General Merrick Garland’s statement that “states may not ban Mifepristone based on disagreement with the FDA’s expert judgment about its safety and efficacy.” Although the Department of Justice has avoided commenting on the specifics of the GenBioPro case, pro-choice legal scholar Rachel Rebouché told The Dispatch that she interpreted Garland’s statement as a nod to a federal “preemption” argument.
“That federal law preempts state law is a constitutional principle,” she said. “One argument is that the FDA regulation of [medication abortion], on the basis of decades of safety and efficacy evidence and as based on its statutory duty to vet the drugs that enter the market, trumps state laws to the contrary.” Although a Massachusetts judge sided with an opioid drug manufacturer in an FDA preemption case in 2014, the concept has been “largely untested in the courts,” Rebouché said.
A state law explicitly banning mifepristone would be “pretty highly likely” to be preempted by FDA authority, Donley said. But so far, states with abortion bans have opted for general bans that don’t specifically single out mifepristone and are thus less vulnerable to the preemption argument. As a result, those states could argue in court that they are not interfering with the FDA’s drug regulation authority.
While GenBioPro argues that states shouldn’t be able to regulate mifepristone more stringently than the FDA does, how stringent those FDA regulations should be in the first place remains an open debate. Pro-life groups have long argued that mifepristone is not as safe and effective as its proponents claim. For example, in a longitudinal study using Medicaid data from 17 states, Charlotte Lozier Institute researchers that found that “chemical abortion is consistently and progressively associated with more postabortion ER visit morbidity than surgical abortion.”
In stark contrast, some pro-choice groups want the FDA to loosen the REMS around mifepristone or eliminate it altogether—Planned Parenthood has called the REMS “a set of unnecessary restrictions.”
Donley—coauthor with Rebouché and David Cohen of a forthcoming Columbia Law Review article exploring the future of “interjurisdictional” conflict over abortion—also believes the REMS is medically unnecessary. But as a pro-choice activist, she is wary of calls to remove it entirely.
“The REMS, ironically, is one of the reasons the preemption argument is … stronger,” she told The Dispatch. The FDA can point to the REMS as evidence that it has “regulated the drug extremely closely in a way that really promotes the idea that its regulation is not just the floor, but is also the ceiling as well.”
“Now that we’re in a post-Dobbs world, if I was speaking like an advocate, and not like a scientist, I would say, remove the most burdensome parts of the REMS … so that you still have a REMS on the book to maintain the preemption argument,” Donley said.
But even modifying the REMS could have other unintended consequences down the road: A future Republican administration would likely attempt to reverse any changes the Biden administration makes.
Regardless of what President Joe Biden decides, the end of Roe’s national standard means the bulk of the abortion fight will take place in the states.




Please note that we at The Dispatch hold ourselves, our work, and our commenters to a higher standard than other places on the internet. We welcome comments that foster genuine debate or discussion—including comments critical of us or our work—but responses that include ad hominem attacks on fellow Dispatch members or are intended to stoke fear and anger may be moderated.
With your membership, you only have the ability to comment on The Morning Dispatch articles. Consider upgrading to join the conversation everywhere.